By a mom who’s been there—with her child, with her heart, and with way too many hospital bags
If you’re reading this, I know you’re in the middle of it—the planning, the anxiety, the endless checklists, and the unknowns. I was there too—not long ago—with my child, who has special needs and faced spinal fusion surgery.
While no one can fully prepare you for how it feels, I’m here to walk beside you and share everything I learned. Because no matter how much you read, it always feels like something’s missing. And sometimes, it’s that one unexpected thing that makes the biggest difference.
So here it is—what actually helped us: the physical, the emotional, and everything in between.
BEFORE SURGERY: PHYSICAL & EMOTIONAL PREP
Talk Less, Show More
Explain surgery in simple, reassuring ways. If your child can handle it, ask the surgeon to show them a rod model—but use your intuition. For some kids (especially those with anxiety or sensory challenges), it’s better after the surgery once fear won’t override logic.
We also:
- Watched YouTube videos of real teens post-surgery
- Used visual aids and checklists
- Encouraged journaling or drawing to process feelings
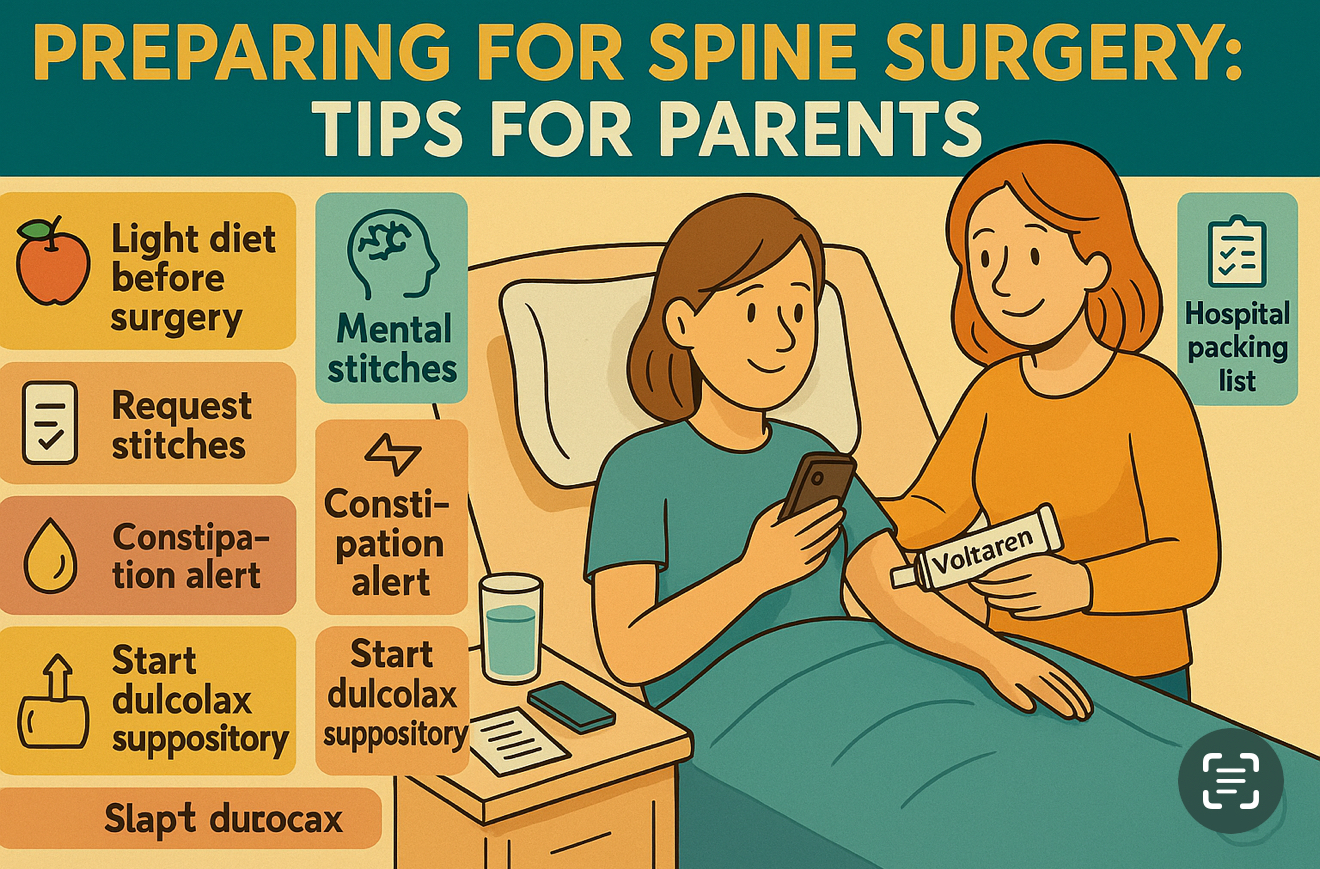
Start Cleaning Up the Diet (Yes, 1–2 Weeks Before)
Especially if your child has Prader-Willi Syndrome or other digestive sensitivities:
- Shift to a light, clean, low-residue diet (soups, soft veggies, lean protein)
- Avoid heavy fats or carbs
- Keep water intake high
- Why? Because digestion slows even more after surgery, and trust me—constipation can be the biggest pain of all.
THE BIGGEST POST-OP ISSUE MOST PEOPLE UNDERESTIMATE: CONSTIPATION
Yes, I said it. And I’ll keep saying it because it needs to be planned for.
Pain meds, anesthesia, fear of movement, antibiotics—it all backs things up.
What helped us:
- Dulcolax suppositories – total game changer
- Probiotics (started before and after)
- Magnesium powder + prune juice
- Simple foods post-op – nothing heavy
- Stool softeners on standby
And I’ll be honest: the constipation was worse than the incision pain. So please don’t skip this prep.
WHAT TO PACK: HOSPITAL BAG ESSENTIALS
Here’s what made a real difference (and what many parents from support groups swear by):
Comfort for Your Child:
- Body pillow (this was GOLD)
- Button-up pajamas (avoid anything you have to pull over the head)
- Favorite robe or hoodie (something familiar)
- Non-slip socks or slippers with backs
- Personal pillow or blanket from home
- Eye mask + earplugs for sleep
- Squishmallow or stuffed animal – they help comfort AND support the knees
For You (the Parent/Caregiver):
- Pillow chair or support cushion
- Long phone charger + multi-outlet plug
- Lip balm, wipes, dry shampoo
- Easy snacks (and tea/coffee if allowed)
Entertainment & Emotional Support:
- Download audiobooks or shows in advance (Wi-Fi isn’t always great)
- Bring something light and uplifting to pass the time
- Small photos or decorations for the room can brighten things up
PAIN MANAGEMENT & HEALING TOOLS
- Don’t be afraid to advocate for pain support.
Ask about:
- Ketamine drip (used initially in ICU)
- Gabapentin
- Muscle relaxers (request these specifically—they really help)
- Tylenol/Oxy as needed
- Voltaren ointment was a true relief for us. I massaged it gently around the back (never directly on the wound) and it helped with tightness and muscle pain.
More importantly, that massage became our bonding time.
I used those quiet moments to play music or listen to audiobooks with my child.
Sometimes the healing comes from the hands that raised them.
IF YOUR CHILD HAS DIABETES (T1)
- Contact the hospital beforehand to check their rules around insulin pumps, CGMs, etc.
- Bring all supplies—backups too. Don’t count on the hospital pharmacy having what you need.
- Be ready to manage blood sugars manually (finger pricks) until hospital clears you for devices.
- Request a note from your endocrinologist outlining your child’s needs and your involvement.
GIRL-TO-GIRL TIP: SURGERY STRESS OFTEN TRIGGERS A PERIOD
Yep. It’s common. Even if she’s not due, the stress and hormones often bring on a period during or right after surgery.
Here’s what helped us be ready:
- Dark underwear
- Pads + wipes (pack more than usual)
- Comfortable, loose clothing
- Quietly talk about it before—especially if it’s one of her first times
AFTER SURGERY: COMFORT, CONNECTION & ROUTINE
- Keep food light and the atmosphere soft.
- Use melatonin or calming techniques at night if needed.
- Expect emotional ups and downs as meds wear off—this is normal.
- Gentle movement (even just sitting up) helps healing.
- Set up a recovery space at home that’s comfortable, accessible, and calming.
A Final Word From Me, Mama to Mama (or Papa)
You don’t have to do everything perfectly. You don’t need a Pinterest-worthy hospital bag.
What your child really needs is you—calm, present, and prepared.
You’ll feel overwhelmed. You’ll cry in the hospital bathroom (I did). But then you’ll come out stronger, because love makes you brave.
And this journey?
You’ll walk it together—one step, one breath, one soft hand on their back at a time.
You’ve got this. And if no one else says it today—I’m proud of you.